By Dr. Allison Hartman
As a prey species, horse evolved to have their eyes located on the side of their head to attain a wider field of vision. While this helps them to better identify potential dangers (mountain lions, bikers, plastic grocery bags, etc) it also predisposes them to injuries specific to their eyes and surrounding structures.
When is it an Emergency?
Ophthalmic emergencies requiring immediate attention from your veterinarian include, but are not limited to:
- Foreign body located anywhere within the eye or surrounding ophthalmic structures (Figure 1)
- Corneal ulcers – usually accompanied by clear or mucoid discharge from the effected eye, squinting, swelling of the eyelids and discoloration (blue, white, yellow, red) of the cornea (Figure 2)
- Corneal lacerations – often results from an encounter with rouge tree branches, hay mangers, bucket hangers and other sharp objects (Figure 3)
- Eyelid lacerations – any damage to the eyelids may result in secondary damage to the cornea from deviated eyelashes, loss of protection, etc. (Figure 4)
- Significant trauma to the bony orbit surrounding the eye (Figure 5)
Indications of an equine ophthalmic emergency include:
- Excessive squinting and/or vertical deviation of the eye lashes
- Swelling of one or both eyelids
- Abnormal discharge from the eye
- The presence of blood vessels on the surface of the cornea (Figure 6)
- Corneal discoloration or loss of transparency (haziness or cloudiness) of the cornea
- Presence of a foreign body in or around the eye
- Sudden loss of vision
- Trauma and drooping lips or ears on the same side as the ocular abnormalities
If there is ever a question of what is ‘normal’, the opposite side of the horse’s head is usually helpful for a quick comparison!
Diagnosing Ophthalmic Emergencies
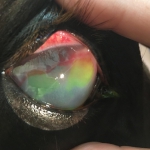
When your veterinarian arrives to assess an ophthalmic emergency, the first step will usually be sedation of your horse to better assess the type, and severity, of ocular trauma. For almost all ophthalmic cases, a neon yellow stain called fluorescein, will be applied to the eye to help visualize any
corneal defects. In most cases, if a defect is present, the stain will bind to the deeper layers of the cornea resulting in a green lesion on the eye. (Figure 7) This green dye will eventually dissipate, but it is key in determining the size as well as the regression of the lesion on subsequent follow up visits. (Keep in mind that there is a nasolacrimal duct that drains excess discharge from the eye into the nose. If you see green dye emerge from your horse’s nose after ocular staining has occurred, don’t be alarmed!! This is perfectly normal).
Other diagnostics may include application of a corneal numbing agent called proparacaine to better palpate the globe and surrounding tissues. If a foreign body needs to be removed, additional numbing techniques may be used to better facilitate the procedure. Once your veterinarian has determined the extent of the damage, they will develop a treatment plan geared specifically towards the needs of your horse.
Treatment of Ophthalmic Emergencies
Ophthalmic treatment plans may include one or more of the following:
- Topical antibiotic ophthalmic ointments – to combat bacterial infections on the corneal surface
- Atropine – results in dilation of the pupil to inhibit spasm of the iris
- Autogenous serum – processed from the horse’s blood, this helps to slow down continued enzymatic breakdown of the cornea.
- Systemic antibiotics – geared towards infections of the eyelids and surrounding structures
- Systemic anti-inflammatories – used to decrease inflammation and pain
Topical treatment of ophthalmic injuries requires multiple applications a day, anywhere from 4-8 times daily! The high number of applications is due to the natural clearing mechanisms of the eye. As an inflamed eye produces more excretions, that excess fluid is flushing the medications from the eye on a regular basis, thus requiring frequent reapplication of medications. For most horses, their
treatment can be managed by the owner in the field. In rare situations, a subpalpebral lavage system may need to be installed for those horses that are highly resistant to direct treatment of the eye (Figure 8).
In most cases, immediate attention to the ophthalmic injury significantly improves the long-term prognosis for the horse. In moderate to severe injuries, follow up appointments and assessments by your veterinarian are key to a positive outcome. These repeat visits are used primarily to determine the efficacy of the current treatment plan and the final duration of therapy. Ophthalmic cases require constant medical attention and diligent follow-up, but a majority of cases have a favorable outcome for you and your horse.
If you think your horse has an ophthalmic emergency, don’t wait a few days to see how he recovers, call your veterinarian now. In severe cases, a few days may be the difference between keeping and losing the eye!